- Home
- Newsletters
- Services
-
Inspirational Features
- The Marcus Family: Equipped with Life Skills Founded in Faith
- A Match Made in Heaven: Revealing the Romantic Heart of God
- The Speirs: A Testimony of God's Redemptive Love
- The Cunanans: Frontliners in the Headlines
- St. Aloysius Gonzaga: The Frontliner of 1590
- From desire to design to destiny: an author’s journey
- Featured Author
- The Power of a Husband-Wife Teamwork
- How Blessings Often Come in Disguised Packages
- Kristin at the Irving Farmer's Market
- St. Patrick's Sunday Refugee Ourreach
- Culinary Medicine
-
Guests Posts
- Transform Your Business Processes for Optimal Performance
- Become a Freelance Writer: 8 Tips for Students and Recent Graduates
- Budget-Friendly Modifications for Your Home Office
- Six Steps to Starting a Startup Successfully
- How to Find Time for Self-Care
- Branding Know-How for the Enterpreneur
- How to conquer web-based projects and uplevel your business
- 5 Proven Ways of Acquiring More Referrals for Your Small Business
- Mental Health
- Making a Comeback
- BLOGS
- Support the Inspired Team
- Fundraisers
|
Having our household receive vaccination provided a lot of relief. For a year, we’ve adhered to protocols even when it wasn’t popular: limited outdoor exposure, wore masks, drastically changed our routines, and ignored advices that didn’t make sense to us. We exercised prudence and faith as we navigated the pandemic. As Dr. Sood would say, “science is merely the systematic study of spirituality.” Now, we can safely enjoy the freedom that vaccination brought, and don’t mind the continued restriction in other aspects. In a battle like this, those who endure to the end have a greater chance at surviving this crisis and emerge victorious. I hope many would. I pray.
0 Comments
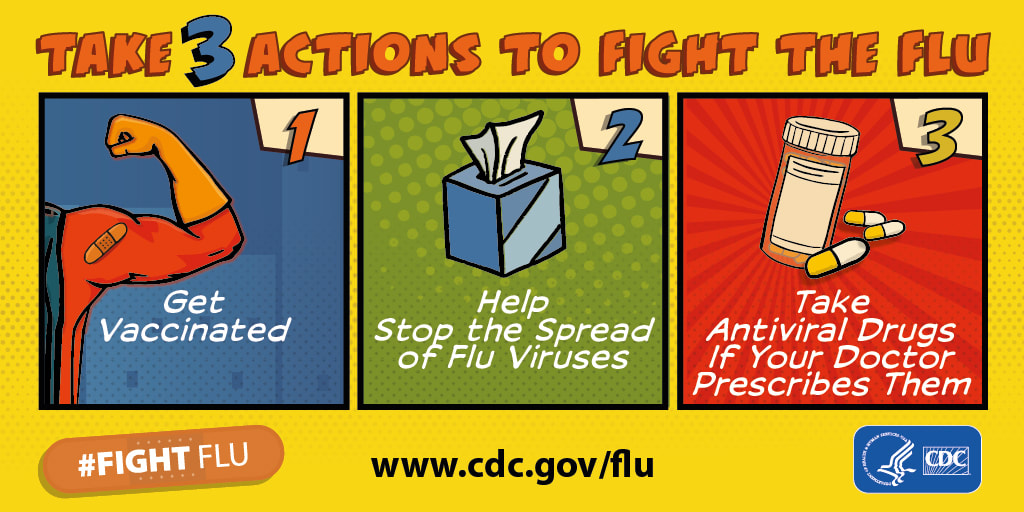
We are at war, and we are the front liners, not the health care workers. They are our last line of defense if we seriously think about it. We land in their arms when we’ve fallen prey, and our immune system succumbs to COVID-19. To hold the line and buy time for the reinforcement—that is, the cure (anti-viral) and prevention (vaccine) to come to our aid, we need to have clear battle strategies and tactics.
‘Tis the season for the flu.
The Centers for Disease Control and Prevention estimates that from October 1, 2019 through January 25, 2020, there have been: - 19 million to 26 million flu illnesses - 8.6 million to 12 million flu medical visits - 180,000 to 310,000 flu hospitalizations - 10,000 to 25,000 flu deaths Here are five steps you can do to fight the flu: 1) Know Your Facts
- oral zinc products - rinsing the nose and sinuses with filtered/treated water (NOT tap water) - honey - vitamin C - probiotics - meditation However, with the flu, there’s little evidence to show effectivity. But if any of these remedies make you feel better, there’s no harm in doing it. Just be mindful that some natural remedies may interact with each other. 2) Take preventive actions to avoid exposure
3) Boost your immunity
4) Stop the spread of the virus
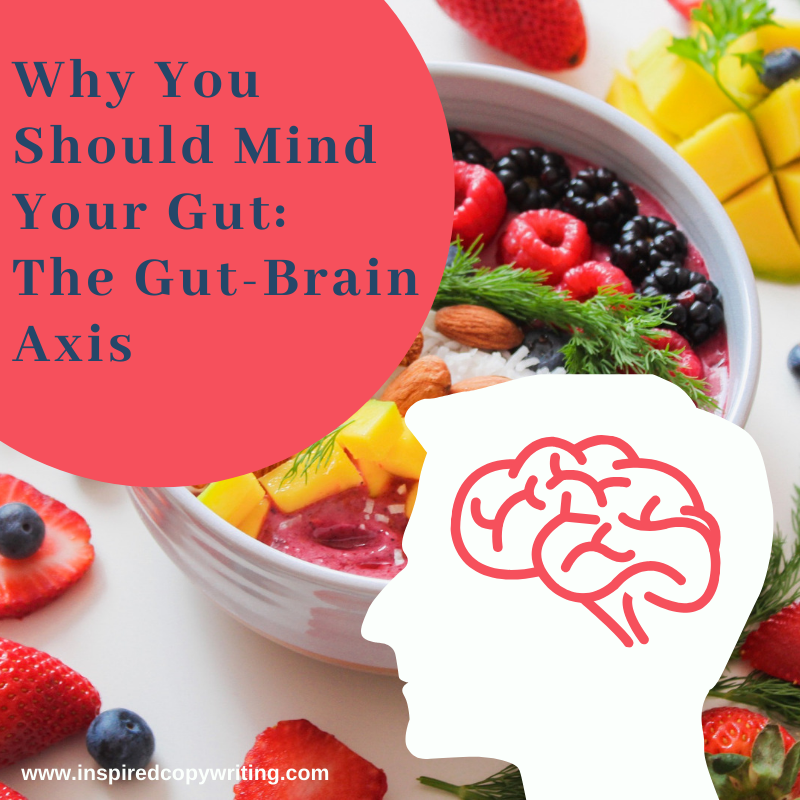
5) Fight Back You may need antiviral drugs (most would not) if you belong to the high-risk group to avoid flu complications like: - pneumonia - sinus and ear infections - inflammation of the heart (myocarditis) - inflammation of the brain (encephalitis), - inflammation of the muscles (myositis), or - multi-organ failure (respiratory or kidney failure). High-risk group includes: - adults 65 years and older - pregnant women - young children and those with neurologic condition - people with asthma, heart disease, stroke, diabetes, HIV/AIDS, cancer Stay well hydrated and well-rested. Flu may be in season but you don’t have to go with the fad. You can be stronger than the flu bug. For more information, visit: https://www.cdc.gov/flu/index.htm https://www.fda.gov/consumers/consumer-updates/rinsing-your sinuses-neti-pots-safe for more information https://www.cdc.gov/flu/resource-center/toolkit/index.htm Lately, I’ve been very forgetful. Is it because of my age, my lifestyle, lack of sleep, or disorganized pace? Or is it my diet? Yes, folks, an exciting finding in recent studies is the connection between our food intake and our brain. Experts call it the Gut-Brain Axis. Does this bring evidence on the table that what you eat becomes you? Could the Gut-Brain Axis solve the missing link on why gaps in nutrition and the microbiome (or bacteria community in your gut) affect your mood and even memory? Trillions of bacteria live in our gut. Apparently, an imbalance occurs when these factors attack our system:
More studies are being done to look at gut-liver, gut-joint, gut-heart, and gut-kidney axes. While researchers are looking for answers, patients with autoimmune disorders have grown frustrated with their pain symptoms. Poor quality of life, dysfunctions, and lifestyle inhibitions, which traditional medicine cannot solve, push them to seek alternative means. Many health providers now factor in their patients’ gut health in managing autoimmune and inflammatory diseases. As a result, the use of prebiotics, probiotics, and even psychobiotics increased in recent years. What other trends do we see? What kind of dietary and lifestyle modifications do experts promote? Here are a few:
People’s gut instincts now lead them to consume more organic, all-natural, fresh farm produce and local products hoping to boost their gut health. They’re minding their guts with more common sense. They start to ask, “Have the get-it-done-fast mentality (fast-food and fast-processing) finally taken its toll on our gut, snagged it, and tore it apart?” Perhaps it’s time to mind our gut and ponder. What’s in your gut? The answer might lead you to the key that could save you from gut-wrenching troubles. REFERENCES:
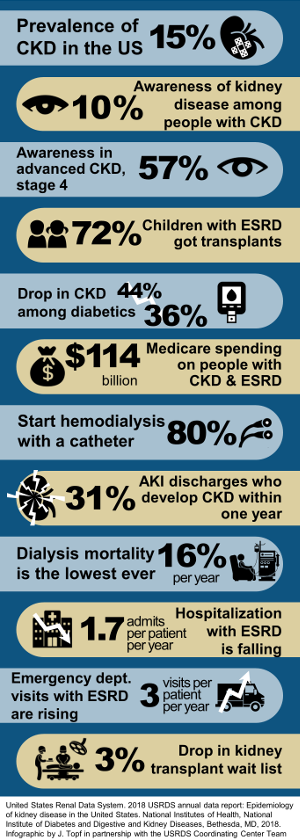
"How could this be? Renal failure? I wish I had known sooner. I could have prevented it. My doctor didn't tell me until it was too late." Nina, a 40-year-old businesswoman looked at me with tears in her eyes. "I didn't understand it...the protein in the urine...because of my hypertension. Why didn't I get tested for this before? Now, I have to do this forever?" She pointed at the dialysis machine beside her, regarding it as a foe rather than a friend. For Robin, a 28-year-old single mother, her dream of finishing college was swept away from the staggering news of renal failure. "I had no idea that my kidneys were getting damaged." She has juvenile diabetes mellitus and didn't have an inkling that renal failure is one of its potential consequences. "I felt bloated. I thought I just gained weight. And then my swollen legs... then the shortness of breath. My doctor told me that I had fluid in my lungs and needed to undergo dialysis immediately. Then they put this on my neck." She pointed at the central venous catheter for dialysis access jutting out in an awkward position below her right jaw. "I don't like my friends to see me like this. And my 3-year-old daughter... she'd be scared." Her voice cracked as she struggled to control her emotion. I've worked for two years as a dialysis nurse and it wasn't uncommon for me to hear patients lament that had they known they were at risk for end-stage renal disease (ESRD), requiring dialysis or kidney transplantation, they would have taken better care of themselves. Diabetes and hypertension still remain as the major causes of ESRD. According to the 2018 Annual U.S. Renal Data System, diabetes ranks first as the primary cause of ESRD for 44% of new patients and 29% had a primary diagnosis of hypertension. For most of these patients, renal failure never entered their consciousness until it slapped them in the face. And most had to deal with hemodialysis, which required a lifestyle overhaul. Dialysis sessions run three to four times a week, lasting three to four hours each visit. The demands on the family resources and the many food and fluid restrictions for the patients make adhering to this new lifestyle a major challenge. The first year of hemodialysis treatment can prove to be a nightmare. Infection of vascular catheter access, blood toxicity, and heart and lung congestion bring the patients back to the hospital time and again. Unknown to most hypertensive and diabetic patients, chronic kidney disease starts to threaten their kidneys from the moment of diagnosis. But the disease progression from CKD to ESRD may take months or years to happen depending on how they control their blood sugar or blood pressure. So, don't get caught off guard like Robin and Nina. You can detect subtle signs and symptoms of worsening CKD and impending ESRD with regular screening and follow-up. How do you monitor your kidney's health? There are the markers that will reveal kidney function:
The plan of management for early stages of CKD focuses on slowing down the disease progression. How?
Your BP goal: If you are 60 years or older: Keep your BP < 150/90 If you are younger (at least 18 years old) or 60 years or older but have diabetes or chronic kidney disease: Keep your BP < 140/90 Your Blood Sugar Goal: Daily blood sugar monitoring tracks the adequacy of your medication and food intake. A blood test called HbA1C can detect poor blood sugar control for the past three months. The desirable level is <7% or an eAG of <154 mg/dL. Get tested every 3-6 months. To meet that goal, your daily blood sugar should be well monitored and controlled. Here are typical targets, which may vary according individual medical needs:
If CKD progresses into kidney failure, you will need a permanent vascular access such as a graft or fistula (typically on your arm). These are less prone to infection. In more than 15 years, the rate of infectious and cardiovascular events in the first year was high because majority of the newly diagnoses patients with ESRD come in without prior detection of CKD. This indicates the need for better monitoring of renal function among diabetics and hypertensives with emphasis on prevention. In general, the following are recommended to delay if not prevent end-stage renal disease:
Don't feel helpless when it comes to your health. There are many resources available to you. These are just a few of them:
Find one that resonates best with you and stick to a lifestyle change program. With greater awareness, you will be able to participate in your health care and prevention of disease complications. You will become more prepared should chronic kidney disease set in and give you more options other than hemodialysis to maintain a favorable lifestyle. |
Archives
April 2021
CategoriesThe above information are from the CDC and posted for educational purposes only, and are not necessarily supported in whole by this site. As with any education material, use discretion and diligence in adopting the practices to your personal condition and lifestyle.
|




 RSS Feed
RSS Feed