Day 24: Lipid Profile and Why It’s High
Tess (not her real name) recently had her lipid profile tested. Although her BMI had always been normal, her lipid profile was always problematic because she was genetically predisposed to cardiovascular disease and diabetes. She claims that she eats a prudent diet, more plant-based and whole foods. But today, she was happy because finally, her triglycerides and LDL are within normal limits. Her cholesterol was still high, but it’s mainly because her HDL (the good cholesterol) is in the 90s, so her doctor said not to worry because she has more good cholesterol than the bad ones that build plaques and cause high blood pressure and stroke.
So we ask Tess what she did that changed her blood levels.
We learned that she had limited her red meat intake (she used to eat mostly lean meat), consumed mostly fish but only 1-2x a week, and decreased her refined carbohydrate intake. She also increased her fiber intake like fruits and nuts, more leafy greens, read the labels, and tried to stick to the 5% saturated fat and added sugar levels and 20% fiber and micronutrients. She ate three main meals with 500 quality calories and three snacks with about 100 quality calories (fruits, nuts, and legumes).
But what she felt made a big difference was the 10-15 min exercise that she added to her routine. She’d walk around the neighborhood or on the treadmill or do the sun-moon-salutation 20 times. The feeling of well-being from the exercise improved her overall mood and decreased her cravings for sweets, which she realized was her way of lifting her spirit when she felt down. She also became more mindful of her water intake. She observed that she craved salty foods when her water intake was low. Drinking about 2.5-3L a day decreased her salt cravings. She used a water bottle that made tracking easy.
Although she had improved a lot, she knew she can do more. A flabby belly was a poor indicator of health and her LDL was still on the high normal side at 97 mg/dL.
Her results included a recommendation for people who are at risk for DM or CVD to keep their LDL cholesterol < 70 mg/dL..
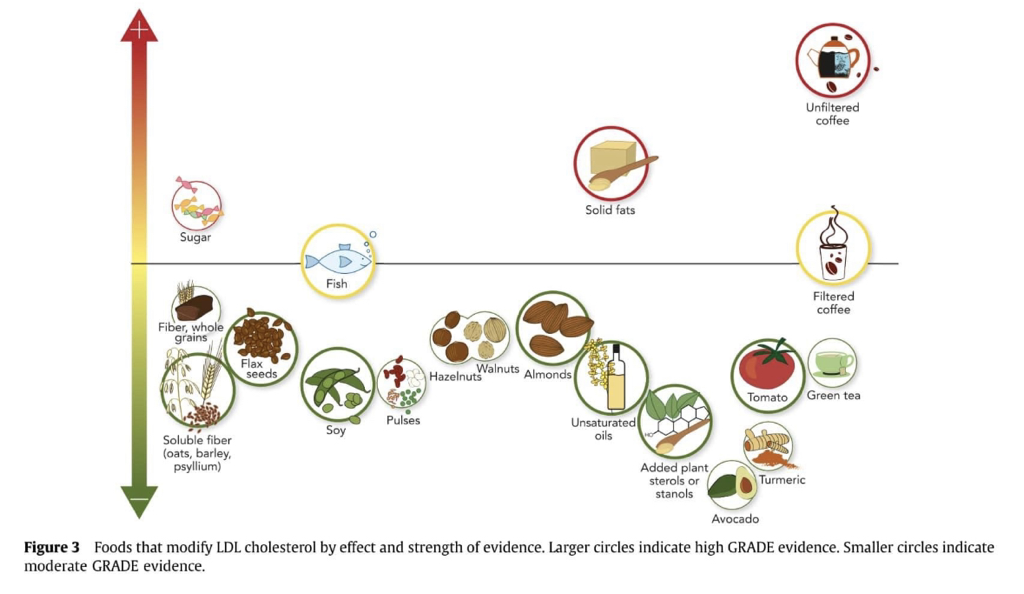
What else can she do to improve her LDL level?
Review the chart below and read the scientific paper.
So we ask Tess what she did that changed her blood levels.
We learned that she had limited her red meat intake (she used to eat mostly lean meat), consumed mostly fish but only 1-2x a week, and decreased her refined carbohydrate intake. She also increased her fiber intake like fruits and nuts, more leafy greens, read the labels, and tried to stick to the 5% saturated fat and added sugar levels and 20% fiber and micronutrients. She ate three main meals with 500 quality calories and three snacks with about 100 quality calories (fruits, nuts, and legumes).
But what she felt made a big difference was the 10-15 min exercise that she added to her routine. She’d walk around the neighborhood or on the treadmill or do the sun-moon-salutation 20 times. The feeling of well-being from the exercise improved her overall mood and decreased her cravings for sweets, which she realized was her way of lifting her spirit when she felt down. She also became more mindful of her water intake. She observed that she craved salty foods when her water intake was low. Drinking about 2.5-3L a day decreased her salt cravings. She used a water bottle that made tracking easy.
Although she had improved a lot, she knew she can do more. A flabby belly was a poor indicator of health and her LDL was still on the high normal side at 97 mg/dL.
Her results included a recommendation for people who are at risk for DM or CVD to keep their LDL cholesterol < 70 mg/dL..
What else can she do to improve her LDL level?
Review the chart below and read the scientific paper.
FAT CHALLENGE #4
Have your lipid profile tested and see where you can improve.